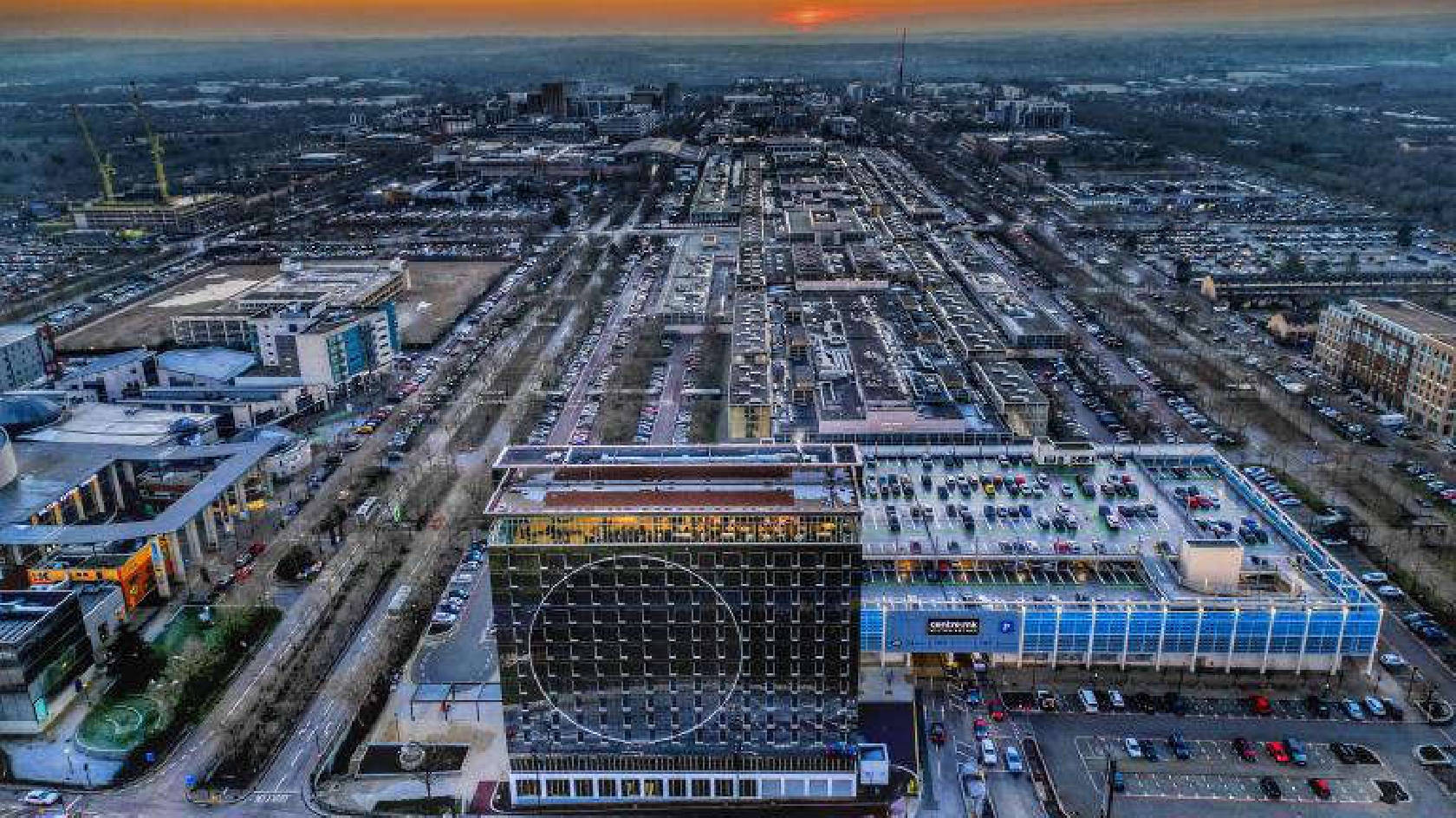
Interest in structured weight management support has increased steadily across Milton Keynes.
Local GP practices and health centres report higher demand from residents seeking clinical pathways rather than informal self-directed attempts. Waiting times have lengthened as more people respond to public health messaging around obesity-related risk and long-term health impact.
This shift reflects a broader change in how weight management is viewed locally. It is no longer framed only as a personal lifestyle matter. Health services increasingly approach it as a preventative and clinical priority, linked to early intervention and system-level planning.
Rising Demand Across Primary Care Services
Primary care teams in Milton Keynes report sustained pressure linked to weight-related conditions. GPs note higher presentation rates for type 2 diabetes, cardiovascular risk factors, joint pain, and sleep apnoea. These conditions frequently appear together, increasing the complexity of patient care.
As demand grows, practices focus on identifying patients earlier and directing them toward structured support, aligning with broader UK obesity healthcare goals aimed at reducing escalation into specialist care while managing workload across primary services.
Local NHS services provide access to weight management programmes for eligible patients. These pathways combine behavioural support, nutritional counselling, and clinical monitoring. Capacity has expanded, but demand continues to outpace availability.
Eligibility Criteria and Referral Pathways
Access to NHS weight management support in Milton Keynes depends on clinical assessment and defined referral routes, reflecting NHS digital weight management eligibility requirements designed to prioritise patients with the greatest clinical need.
Referral processes have been refined to improve efficiency. However, limited awareness of eligibility requirements can delay access, particularly for patients unfamiliar with formal healthcare pathways. In some cases, individuals engage with services only after symptoms have progressed.
Clear communication between patients and primary care teams remains essential. Accurate medical records and consistent follow-up support appropriate referral decisions and reduce unnecessary delays.
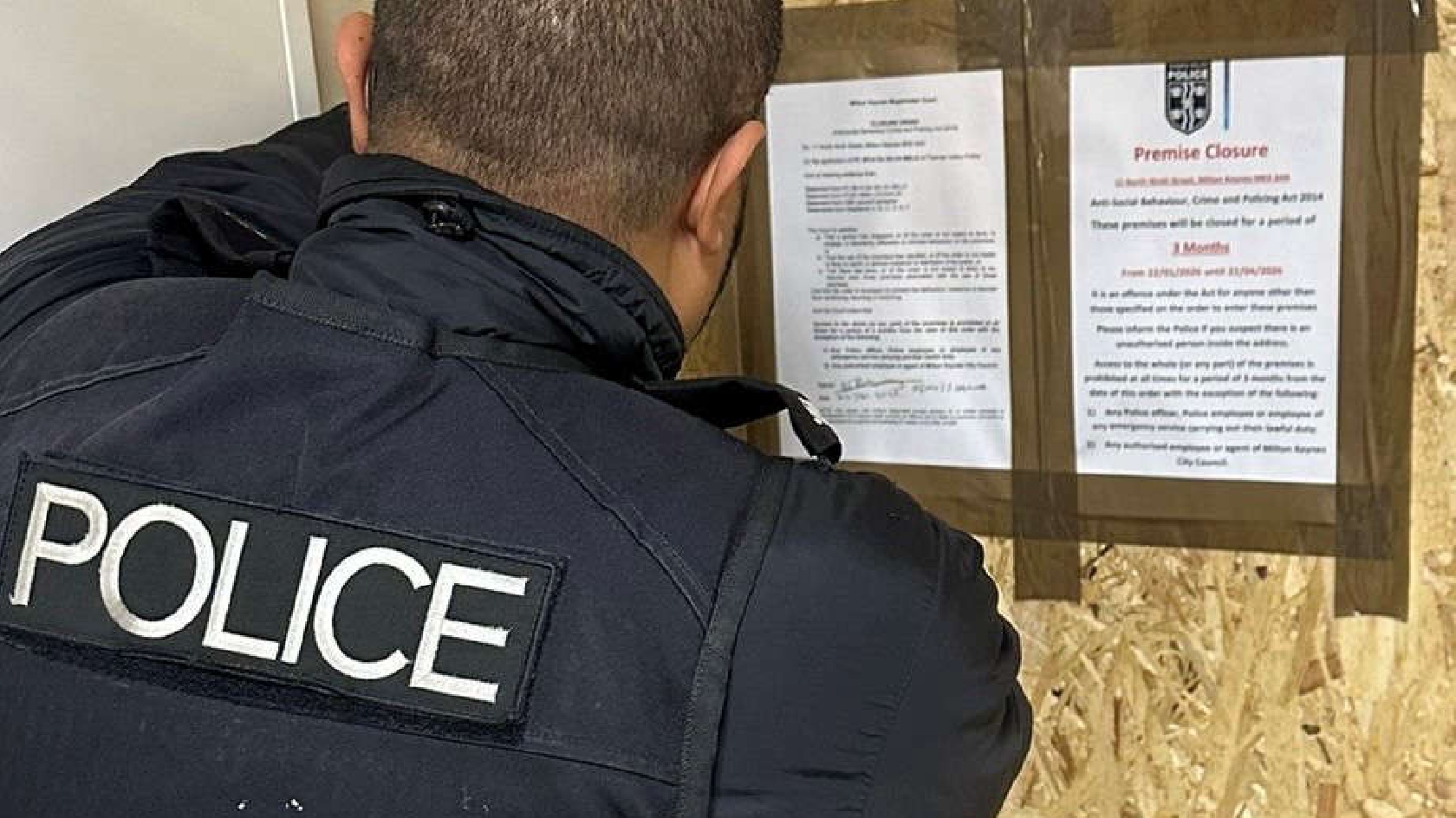
Clinical Weight Management Within a Regulated Framework
Lifestyle adjustment remains the foundation of weight management care. Nutritional balance, physical activity, and behavioural consistency form the baseline for long-term progress. For some patients, these measures alone do not deliver sufficient clinical improvement.
In such cases, medical pathways allow for prescription-based support when strict criteria are met. Treatments including wegovy injections may be considered as part of a broader clinical plan, following assessment and under ongoing supervision. Their role is to support appetite regulation and metabolic control alongside continued lifestyle measures.
Access to prescription treatment requires structured review. Clinical oversight ensures correct use, appropriate duration, and alignment with wider health objectives. This framework reduces misuse and positions medication as a supportive element rather than a standalone solution.
The Role of Regulated Providers
Regulated pharmacies and clinical providers support weight management pathways by linking treatment access to medical assessment. This structure reinforces safety, accountability, and continuity of care.
Patients receive clear monitoring schedules and review points aligned with clinical standards. Regular assessment allows healthcare teams to track progress, manage side effects, and adjust plans where needed.
This regulated approach strengthens outcomes by integrating medication into a wider healthcare framework rather than isolating it from primary care oversight.
Community and NHS-Supported Programmes
Alongside clinical pathways, Milton Keynes residents access community-based and NHS-supported programmes. These services focus on sustained engagement rather than rapid outcomes. Group-based formats provide routine, accountability, and peer reinforcement.
Health professionals track progress using standard clinical measures, including weight trends, blood pressure, and metabolic markers. Regular check-ins support gradual improvement and help participants maintain engagement over time.
Evidence from local services suggests that consistent participation plays a greater role in outcomes than programme format alone, a pattern also observed in community weight management trial outcomes that assess engagement and adherence over time.
Digital and Hybrid Support Models
Digital health tools increasingly complement in-person services across Milton Keynes. App-based programmes and remote monitoring options extend support between appointments and reduce reliance on face-to-face contact alone.
Hybrid models combine digital tracking with scheduled clinical reviews, an approach already reflected in NHS hospital weight management services where continuity and professional oversight remain central to long-term progress.
Healthcare teams emphasise that digital tools function best when integrated into structured care plans. Standalone use without clinical context offers limited long-term benefit.
Integrated Care and Long-Term Outcomes
Weight management outcomes improve when services operate within coordinated frameworks, a pattern reflected in long-term outcomes in integrated obesity care where consistency and accountability support sustained clinical impact.
Local health planners continue refining service delivery models to reflect rising demand. Efforts focus on clearer referral coordination, improved patient communication, and balanced use of clinical and community resources.
This integrated structure supports both individual outcomes and system sustainability.
Weight management in Milton Keynes is increasingly shaped by structured care rather than isolated effort. When lifestyle support, clinical oversight, and regulated treatment operate together, outcomes become more sustainable for both individuals and services. Clear pathways and consistent engagement help residents move from short-term attempts toward long-term health stability.